Lymphatic malformations are rare but potentially life-altering conditions in which lymphatic vessels grow abnormally. These malformed vessels can cause swelling, pain, breathing problems, or disfigurement, often starting early in life. For families, patients, and doctors, managing these conditions has long been a challenge, partly because the root cause is often hidden deep in the patient’s cells.
One key reason? Mosaic mutations. These are mutations that exist in only a small number of cells, making them incredibly difficult to detect using standard genetic tests. But a new research platform is changing that.
From Patient Biopsy to 3D Mini-Tissue
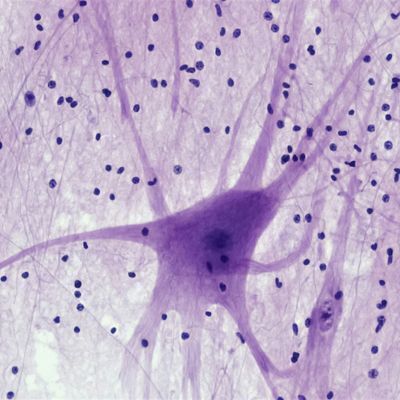
In a groundbreaking new approach, scientists have developed a "biopsy-to-bench" system that starts with a small tissue sample from a patient. They use this sample to grow 3D lymphatic organoids — tiny, lab-grown models that mimic how the patient's lymphatic tissues behave in real life.
These organoids allow researchers to:
- Study cells that carry rare mosaic mutations
- Use deep genetic sequencing to uncover hard-to-find mutations in genes like PIK3CA, KRAS, and HRAS
- Test how different tissues react to medications like Alpelisib and sirolimus
- Monitor tissue behavior in real time with advanced, label-free imaging systems
What They Found
Hidden Mutations Revealed
By using deep sequencing on these organoids, researchers were able to identify mosaic mutations that are usually missed in routine genetic testing. This discovery helps explain why some patients with lymphatic malformations don’t show any detectable mutations in traditional genetic tests.
Different Behaviors, Different Drugs
Not all lymphatic tissues react the same way to treatments. In the lab, scientists observed how diseased organoids responded differently to drugs compared to healthy ones. For example, some showed a strong response to Alpelisib, a drug that targets the PIK3CA pathway, while others responded better to sirolimus, which affects a different pathway.
Predicting the Best Treatment
Because these organoids are made from a patient’s own tissue, they act as a preview of how that patient might respond to certain treatments. This means doctors could one day test treatments in the lab before prescribing them in real life — a major step toward precision medicine.
Why This Matters
For families and patients facing the uncertainty of a rare lymphatic condition, this research could lead to:
- Faster, more accurate diagnoses
- Better treatment choices with fewer side effects
- A reduced need for trial-and-error in care plans
For scientists and clinicians, it provides a powerful model for studying these diseases and testing new treatments safely and effectively.
A Personalized Future
This biopsy-to-bench platform is more than just a lab technique — it’s a window into the future of personalized medicine. By turning a small tissue sample into a powerful research tool, scientists are getting closer to answers that can directly impact a patient’s life.
Take from the Research Network Seminar presented by Yarelis Gonzalez-Vargas, PhD, From Biopsy to Bench: Engineering Human Lymphatic Tissues for Precision Medicine in Pediatric Vascular Anomalies