Diagnosis
Based on clinical characteristics, radiologic imaging, and pathologic findings, the International Society for the Study of Vascular Anomalies (ISSVA) created a standardized classification system in 1996, broadly categorizing vascular anomalies as tumors and vascular malformations. The ISSVA classification system was recently updated and can be accessed at https://www.issva.org/classification.
Initial presentation of CLA is variable, and the provider needs to have a high index of suspicion for and familiarity with these conditions to provide timely diagnosis and appropriate management. When in doubt referral to a specialized vascular anomalies center should be considered.
Imaging:
Radiologic evaluation should include chest, abdomen, pelvis, and total spine imaging with CT and/or MRI. If there is a suspicion of GSD, then skull imaging is indicated. A skeletal bone survey may be used to focus imaging needs. Dynamic, contrast-enhanced MR lymphangiography can also be helpful in certain situations.
Laboratory Evaluation:
Laboratory investigation should include complete blood count with differential, D-dimer, fibrinogen, prothrombin time (PT), partial thromboplastin time (PTT), albumin and total protein, immunoglobulins, liver and renal function tests, electrolytes, and bone turnover markers (alkaline phosphatase, C-telopeptide, etc.). Recently, angiopoietin-2 (ANGPT 2) have been identified as serum biomarkers in KLA and may be helpful in diagnosis and monitoring treatment response, especially to Sirolimus. (ANGPT 2 testing)
Genetic Testing:
Since mutations in CLA are often somatic, genetic testing of the affected tissue, not peripheral blood, should be considered to guide therapy. Biopsy of a soft tissue lesion is recommended over bone biopsy. Biopsy of ribs and vertebrae should be avoided as these can result in persistent pleural effusions and CSF leaks. Genetic testing of circulating free DNA (cfDNA) in blood and effusions is emerging as a potential diagnostic aid (spotSeq).
Treatment
Most patients with CLAs have extensive and invasive disease burden, necessitating systemic therapeutic approaches. Originally there was not a clear understanding of the underlying pathobiology and so medical therapies for patients with CLAs focused on agents that interfered with known mechanistic pathways such as angiogenesis (interferon-alpha, radiation) or the function of specific cells involved in disease pathogenesis such as LEC (mTOR and VEGF inhibitors) and osteoclasts (bisphosphonates). Symptom control has been the goal of treatment.
Recent advancements have identified pathognomonic gene variants occurring in low allelic frequency in a growing number of patients with CLAs.3 As a result, targeted medical therapies based upon identified gene variants are central to managing these diseases (reference 12) Many of the identified genetic variants in CLA patients are similar or identical to those identified in many cancers, offering significant potential for drug repurposing.
Medical Therapies:
Medications that have been commonly used to treat CLAs include the following (reference 13):
mTOR inhibitors (Sirolimus/Rapamycin)
- A serine/threonine kinase in the PI3K/AKT/mTOR signaling pathway.
- Reduction of mTOR signaling decreases the proliferation and function of the LECs in CLAs.
- Can be used to treat GLA, GSD, CCLA, KLA
- First-line therapy for KLA and studies have found that treatment results in a decrease in serum Ang-2 levels
- Originally approved as an immunosuppressant in 1999
- Dose is approximately 2 mg daily for adults and 0.8 mg/m2 twice daily for children, adjusted to target sirolimus blood concentrations of 8-12 ng/mL.
MEK inhibitors (Trametinib, Selumetinib)
- Block MEK and so cause reductions in ERK activation in the RAS/MAPK signaling pathway.
- Has been used to treat some individuals with GSD, KLA, and CCLA, although no clinical trials to date.
- Various levels of therapeutic improvement but has been observed in the remodeling of the lymphatic system and subsequent improvement of symptoms.
PIK3CA inhibitor (Alpelisib)
- A p110a-specific PI3K inhibitor.
- Used for the treatment of PIK3CA-mutated breast cancer.
- Has been used to treat PIK3CA related overgrowth spectrum (PROS).
- Has been shown to reduce organ dysfunction and improve vessel normalization.
- Effective at decreasing lesions related to CLAs.
AKT inhibitor (Miransertib)
- Targets AKT in PI3K/AKT/mTOR pathway.
- Has been successful in treating some PROS patients and is being investigated as a cancer therapeutic.
- Decreases cell proliferation resulting from activation of the PI3K/AKT/mTOR signaling pathway.
Bisphosphonates (Zoledronic acid, Pamidronate)
- Bisphosphonates slow bone resorption by reducing osteoclast function, improving bone mineral density.
- Nitrogen-containing bisphosphonates affect the RAS/MAPK pathway by reducing isoprenylation and subsequent activation of small GTPases.
- Has been used for the treatment of GLA, GSD, and KLA, as a single agent and in combination with Sirolimus.
Interferon-alfa 2B
- Interferon-alpha 2B has been reported to reduce lymphangiogenic activity as a single agent and in combination with zoledronic acid.
Surgery/Interventional Radiology
Surgical resection, sclerotherapy, and laser therapy can provide local control and symptomatic relief to CLA patients with recurrent effusions, infections, and pain. Surgical resection is often not possible due to the localization and extent of the lesions. Minimally invasive, image-guided procedures such as sclerotherapy, embolization, and recanalization can sometimes be used, but as the lesions are often extensive and located in challenging locations, these procedures can be difficult. Lymphovenous anastomosis, an innovative microsurgical technique developed to correct lymphedema, is being used more frequently to treat CCLAs (reference 14)
Nutrition
- Patients with chylous (lymph fluid with fat) effusions may be prescribed a low-fat diet.
- Patients treated with Sirolimus or Alpelisib may be prescribed a low carbohydrate diet as both medications can raise blood sugar.
Summary Diagnosis and Management
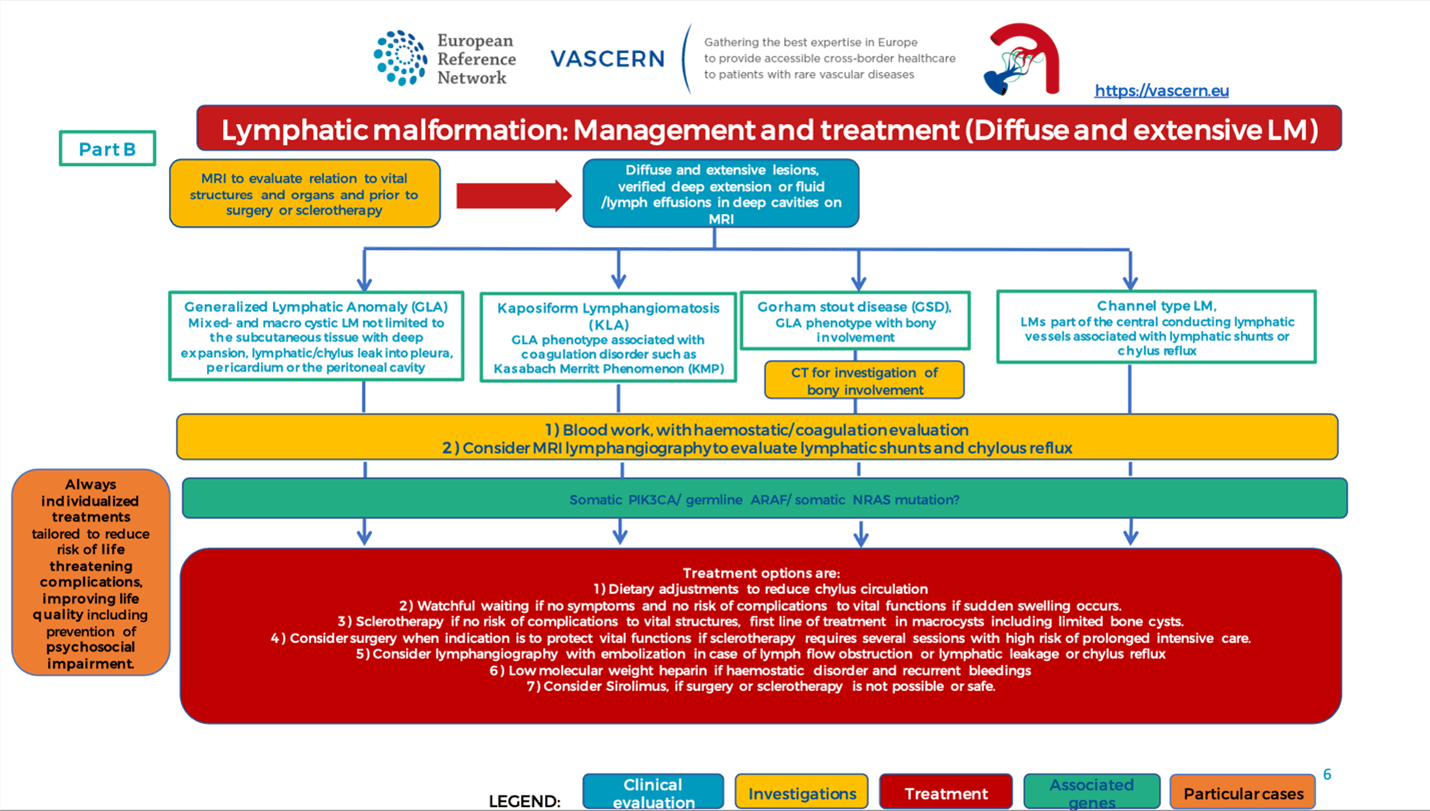
The Vascular Anomalies Working Group (VASCA-WG) of VASCERN developed a diagnostic and management pathway for complex lymphatic anomalies (reference 15). Below is the summary care pathway developed and published by VASCERN.
Figure 13: Diagnostic and Therapeutic Summary (click on image for download)